What Causes Dry Mouth? Know the Symptoms and the Solutions

Dry mouth, cotton mouth, the pasties – no matter what you call it, the feeling that there’s no moisture in your mouth is unpleasant and uncomfortable. Experiencing a dry mouth is normal from time to time, and about half of the population experiences it to some extent during their lifetimes. It can range from a minor annoyance to a potentially serious issue.
The medical term for dry mouth is “xerostomia,” and it describes that feeling when your mouth doesn’t have enough saliva in it to stay moist. When you’re experiencing it, normal behaviors like swallowing or even talking can become difficult.
If you get dry mouth occasionally, there’s probably no reason to worry; however, chronic dry mouth can be a sign of another medical condition, or it can lead to its own problems down the road.
What Causes Dry Mouth?
The causes of dry mouth range from simple situations or behaviors – like feeling stressed or nervous or primarily breathing through your mouth – to more complicated underlying issues. These could be:
- Taking medications, including antihistamines, antidepressants, muscle relaxants, and blood pressure medication
- Nutritional deficiency, especially zinc and vitamin B
- Sjogren’s Syndrome, which is an immune system disease that affects the mucous membranes and causes dry mouth and dry eyes
- Diseases that affect your connective tissues, like lupus, sclerosis, or rheumatoid arthritis
- Receiving chemotherapy or radiation treatment for cancer
- Chronic conditions like autoimmune disease, hepatitis, HIV, depression, anxiety, or diabetes

Dry mouth is a common complaint amongst the elderly, and scientists once thought it was a natural consequence of aging. However, studies have shown that there’s nothing about aging to indicate that it causes dry mouth.
Now, researchers believe that the older you get, the more likely you are to have experienced health conditions, treatments (like chemotherapy), or to be taking medications that lead to dry mouth.
Xerostomia vs. Salivary Gland Hypofunction (SGH)
Xerostomia is a subjective condition, and the term applies specifically to the feeling that your mouth is too dry. This feeling can vary from person to person, and at this time, there’s no way to measure or compare the dryness among those who experience it – although some studies have tried unsuccessful tactics like taking pictures of the tongues of people who have dry mouth.
When patients complain of xerostomia, doctors currently attempt to assess the severity by asking questions to the person who’s experiencing it.
In addition to xerostomia, there is another dry mouth condition known as salivary gland hypofunction, or SGH. SGH refers to how much saliva your glands are actually producing, so unlike xerostomia, SGH can be measured.
How SGH Is Measured
Doctors can either stimulate your three major saliva glands with citric acid or a piece of paraffin, or they can measure your saliva production without any stimulation to get an idea of how dry your mouth is on a normal basis.
But is SGH connected to or a cause of xerostomia? After all, if you feel like you have dry mouth, logic seems to dictate that your salivary glands are probably not making enough saliva.
Surprisingly, research has found that they’re actually separate conditions, and they rarely occur simultaneously. Xerostomia is experienced by as many as 42% of people and SGH has been reported by up to 47%, but both conditions happen together in just 2% to 6% of people.
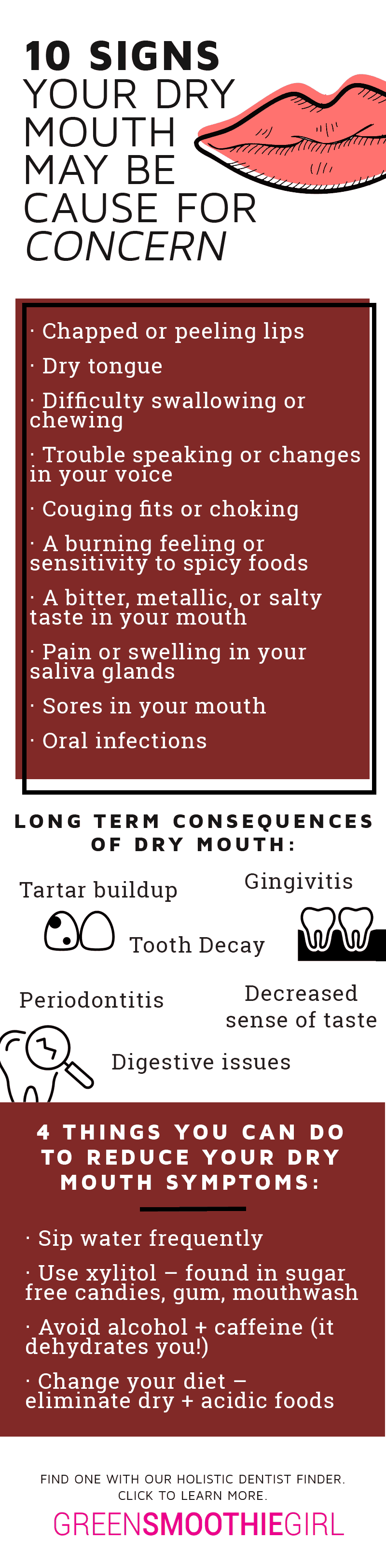
Dry Mouth Symptoms and Signs
No matter what causes dry mouth, the symptoms are similar. If you’re experiencing xerostomia or you’ve been diagnosed with SGH, you may experience some of these common signs and symptoms:

- Chapped or peeling lips
- Dry tongue
- Difficulty swallowing or chewing
- Trouble speaking, or changes in your voice
- Coughing fits or choking
- A burning feeling or sensitivity to spicy foods
- A bitter, metallic, or salty taste in your mouth
- Pain or swelling in your saliva glands
- Sores in your mouth
- Oral infections
While most of these symptoms seem to be minor, they can take a toll on the person experiencing them, and can lead to more serious consequences down the road.
Long-term Effects of Dry Mouth
Over time, dry mouth can affect your oral health as well as your overall health. When you don’t have enough saliva to neutralize the acids in your mouth that come from foods you eat or are are created by bacteria, those acids can pull minerals out of your teeth.
When those minerals are pulled out of the teeth, the teeth are weakened and severe tooth decay can rapidly occur. Tarter may also increase, which can lead to gingivitis and more serious gum disease. This is an overall health concern because gum disease has been linked to other health conditions, like cancer and heart disease.
Saliva also affects your ability to taste, so constant dry mouth can interfere with your ability to enjoy food. It also aids in digestion by helping to break down food while it’s in your mouth, and by providing digestive enzymes that help your body process starch. Dry mouth can eventually cause digestive issues as your body becomes less able to break down foods.
Managing Dry Mouth
Managing dry mouth largely depends upon what’s causing it. If you’re experiencing medication-induced dry mouth, your doctor may try to adjust your prescriptions to reduce the effects. If it’s a side effect of a disease, a dry mouth gel or spray that acts as a saliva substitute may be able to provide relief. There are also medications that can be prescribed to stimulate saliva glads to give you a more moist mouth.
If you have dry mouth, there are things you can do to reduce your symptoms. Experts recommend:
- Sipping water frequently, which can moisten your mouth and wash away bacteria
- Oil pulling, to neutralize bacteria and moisten oral tissues
- Avoiding alcohol and caffeine, which can dehydrate your body
- Changing your diet to eliminate dry or acidic foods
- Add foods rich in B vitamins and zinc, since deficiency in thse nutrients is a common cause of dry mouth
If your dry mouth becomes chronic, a biological dentist may be able to help you further with more targeted solutions:
- Find the underlying cause and can suggest alternative solutions to help you manage it – like how to change your diet, avoid toxins, or address an underlying disease.
- Perform a salivary gland rejuvenation procedure through a special neural reset injection with an anesthetic called Procaine.
Even if it’s just a minor inconvenience, it’s important to control dry mouth sooner rather than later. Not only can you prevent tooth decay, choking, and other serious issues down the road, but you’ll pave the way for a better quality of life.
Need to find a biological dentist near you? Use our free Holistic Dentist Finder to locate one today!

Robyn Openshaw, MSW, is the bestselling author of The Green Smoothies Diet, 12 Steps to Whole Foods, and 2017’s #1 Amazon Bestseller and USA Today Bestseller, Vibe.
This article was reviewed and approved by Dr. Michelle Jorgensen, DDS, FAGD, TNC, and dental advisor for GreenSmoothieGirl.com. The information included here is not a replacement for professional diagnosis or treatment; please consult a holistic dental professional.
Find natural biological dentists near you, and see at a glance what services they provide, with our free Holistic Dentist Finder. No dentist paid or joined an organization to be included, because it’s not advertising–it’s about you finding the best nontoxic dental services for yourself and your family.
Disclaimer: This article may contain affiliate links, which allows you to support our mission (as well as demonstrate market demand for safer products) without costing you extra.
Sources:
1. Ngo Di Ying Joanna, William Murray Thomson, Dry mouth – An overview, Singapore Dental Journal, Volume 36, 2015, Pages 12-17 https://www.sciencedirect.com/science/article/pii/S0377529114200198
2. The Mayo Clinic. “Sjogren’s Syndrome” Retrieved from: https://www.mayoclinic.org/diseases-conditions/sjogrens-syndrome/symptoms-causes/syc-20353216
3. C. Bots, A. Beest, H. Brand The assessment of oral dryness by photographic appearance of the tongue Dent. J., 217 (2) (2014), p. E3
4. Hopcraft MS, Tan C. Xerostomia: an update for clinicians. Aust Dent J. 2010 Sep;55(3):238-44; quiz 353.
5. Gerdin EW1, Einarson S, Jonsson M, Aronsson K, Johansson I. Impact of dry mouth conditions on oral health-related quality of life in older people. Gerodontology. 2005 Dec;22(4):219-26.
6. The Family HealthGuide. “What causes dry mouth — and what treats it” Harvard Health Publishing, 2003. Retrieved from: https://www.health.harvard.edu/diseases-and-conditions/what-causes-dry-mouth-and-what-treats-it-the-family-healthguide
7. National Institutes of Health: Medline Plus. “Dry Mouth” Retrieved from: https://medlineplus.gov/drymouth.html
Mathews Marc J, et al. Oral health and coronary heart disease BMC Oral HealthBMC series – open, inclusive and trusted. 2016 16:122
8. Ngozi N. Nwizu et al. Periodontal Disease and Incident Cancer Risk among Postmenopausal Women: Results from the Women’s Health Initiative Observational Cohort. Cancer Epidemiol Biomarkers Prev; 26(8); 1255–65
Posted in: Dental Health












No comments found, but you can be our first!