What REALLY Causes Gum Disease? A Holistic Dentist Explains

Dr. Michelle Jorgensen, DDS is my own holistic dentist, with whom I created the Healthy Mouth, Healthy Life video masterclass. I’m thrilled to have her guest posting today. –Robyn
This article is excerpted from Dr. Jorgensen's new holistic dental guide book, "Healthy Mouth, Healthy You: Transforming Your Whole-Body Health Starts In The Mouth," and reprinted on GreenSmoothieGirl with permission.
Gum disease isn’t just mouth disease. Gum disease is whole body disease. There have been hundreds of research articles over the last 40 years showing the connection between gum health and overall health, and it’s time you know what all that research has been showing!
The traditional way of thinking about the cause and effect of gum disease is simple. If you don’t brush and floss your teeth often or effectively enough, plaque sticks on the teeth, causes the gums to get inflamed and the gums and bone around the teeth recede. Now, don’t get me wrong. That is still correct in some people and in some situations. However, it is only the tip of the iceberg in regard to what causes gum disease, how you can prevent it, and the damage it leads to if untreated.
In this post:
- What Is Gum Disease? Gingivitis vs. Periodontitis
- What Causes These Gum Diseases?
- How Does Gingivitis Progress To Periodontitis?
- Overall Health Effects of Periodontal Disease
- How Is Gum Disease Diagnosed?
- How Do Holistic Dentists Treat Gum Disease?
- Nutrition and Supplementation for Gum Disease Treatment
What Is Gum Disease? Gingivitis vs. Periodontitis
Let’s start with the basics. There are two basic categories of gum disease: Gingivitis and Periodontitis.
Gingivitis – the official name for the gums is "gingiva." And "itis" always means inflammation. So gingivitis means inflammation of the gums. This is the early stage of Gum Disease where the gums bleed easily and are swollen, but the disease has not progressed to the jawbone.

If you notice that your gums are bleeding, it may be a sign that you have gum disease.
Periodontitis – Your tooth is connected to the jawbone by a ligament called the periodontal ligament. This type of gum disease is inflammation of the periodontal ligament and the bone beneath. Periodontitis is inflammation of the bone and the gums. This is stage 2-4 gum disease when the disease has progressed into the bone and there has been early to advanced bone loss, threatening the tooth and your overall health
What Causes These Gum Diseases?
Bacteria: The bacteria in your mouth like to congregate together. They live in the sticky substance on your teeth and tongue called plaque. The longer they stay in one place, the stickier these colonies get and more bacteria can join them. Just as in any large city, the more bacteria that crowd together, the more garbage they create. It's the garbage (toxins) that inflame the gums.
Pay attention to where the plaque sticks. You’ll see it’s right around the gumline. If the plaque stays there for longer than a few days, the toxins start to damage the fragile gum tissue. Your body, always on guard, sends its warriors there to battle this attack. That's what inflammation is, simply your body's reaction to a foreign invader. This inflammation around the gumline is called gingivitis.
Nutrition: There is another component to gum disease that has very little to do with bacteria. Early in the 19th century, sailors were stricken with scurvy as they sailed across the ocean with a very limited diet. One of the most prominent symptoms of scurvy is bleeding gums and loose teeth.
What was missing in these sailor's diets? Vitamin C.1 If a Vitamin C deficiency could create a disease condition in the gums and bone, it's obvious that nutrition plays a part in gum and bone health.
[Related: How To Find A Good Biological Dentist: 10 Questions to Ask]
Other Causes of Gingivitis and Periodontitis
While bacteria and nutrition are the primary cause of gum disease, there are other factors that contribute. These include:
- Hormonal changes, such as those occurring during pregnancy, puberty, menopause, and monthly menstruation, make the blood supply in the gum tissues more inflamed and the gums are more prone to bleeding and soreness.
- Illnesses may affect the condition of your gums. This includes diseases such as cancer or autoimmune disease that interfere with the immune system. Diabetes affects the body's ability to use blood sugar, so patients with this disease are at higher risk of developing infections, including periodontal disease and cavities.
- Medications can affect oral health, because some decrease the flow of saliva, which has a protective effect on teeth and gums. Some drugs, such as the medication for epilepsy called Dilantin and some heart medications can lead to overgrowth of gum tissue.
- Bad habits such as smoking make it harder for gum tissue to repair itself.
- Family history of dental disease can be a contributing factor for the development of gingivitis.
How Common is Gum Disease?
The startling fact is that more than 50% of the adult population in the US has some level of periodontal disease. That means that one out of every two people have this infection. If left untreated, it can lead to inflammation and disease throughout the body.3

Chronic bad breath is a common symptom of gum disease.
Does Gum Disease Hurt?
Although most adults have some level of gum disease, very few people know it's there.4 Gingivitis is usually not painful. The gums turn red, they bleed when you brush, but they often don't hurt. The early warning system of pain is missing for this disease, which makes it more dangerous.
How Does Gingivitis Progress To Periodontitis?
If the plaque stays there long enough, excess calcium in the blood starts to combine with the plaque and a hard substance called calculus or tartar is formed on the teeth. Now the bacteria are really happy! The calculus is like condos for those bacteria to live in. You can't brush tartar off, so they can live there a long time, continuing to drop their garbage onto the gums.
After a while, the immune system figures out that this invader isn't going away, so it tells the gums to retreat. The periodontal ligament starts to come loose from the tooth, and the gums start to recede down the tooth. This opens up a pathway for the bacterial toxins to get to the bone beneath, which causes the bone to get infected and to start to recede as well. The gums are lost, the bone is lost, and eventually the tooth gets loose and can come out.
What a sorry tale! And most of it happens with no pain. I've often called periodontal disease the silent and deadly killer of teeth.
Symptoms of Periodontitis
Some warning signs of periodontitis are bleeding gums when you brush, a bad taste in your mouth, loose teeth and bad breath. If you have any of these symptoms of advanced gum disease, run, don't walk to the dentist! You don't have any time to lose!
Overall Health Effects of Periodontal Disease
Periodontal Disease is not something to wait on, because decades of scientific research have connected periodontal (gum) disease with other diseases, including diabetes, high blood pressure, heart attacks, stroke, kidney and lung disease, cancer, infertility, erectile dysfunction, preterm birth, and other pregnancy complications.5-14

How Is Gum Disease Diagnosed?
Gum Exam
The health of your gums and bone should be measured at every tooth cleaning, or what we dentists call your “wellness visit”. There is a natural pocket between the tooth and gum that is 2-3 millimeters deep. A special measuring tool is placed in this pocket to measure the depth of it. If it is deeper than 3 millimeters, that is a sign that disease has ALREADY happened.
Bone has already been destroyed and the disease has progressed and has caused or is causing damage NOW. You should not wait to begin treatment as each day leads to further effects in the mouth and in the body.
Other Possible Explanations For Gum Disease Symptoms
There are some health conditions that can mimic gum disease. If the bleeding gums and/or loss of bone is only in certain localized areas, it is very possibly a tooth problem. Have your holistic dentist check:
- Defective dental restorations
- High electric current (galvanism) from metal restorations
- Bite problems
- Mercury fillings in the area.
If the gum disease is more generalized but your teeth are “clean” we will check for health problems, including:
- Depressed immune system
- Low Vitamin C
- Poor diet
- Prescription drug problems
- Hormone imbalances
- pH problems in the gut
How Do Holistic Dentists Treat Gum Disease?
Mechanical cleaning– the bacteria in your mouth creates a sticky layer on your teeth that, if not removed, calcifies and forms tartar that can’t be removed on your own. This tartar harbors other, more dangerous bacteria, and has to be removed if your gums and bone are to return to health.
The official name for this treatment is Scaling and Root Planing, and is what is traditionally prescribed if you are diagnosed with gum disease. This cleaning can be done with traditional hand instruments, or with specialized ultrasonic instruments. Both can be utilized to remove all of the hard deposits on your teeth so your gums can heal.
Laser Cleaning and Disinfection– Laser light energy is used to kill microbes over a large area of the infected root, gum tissue and bone. This laser light is tuned into the harmful bacteria in the infected tissue, and up to 99.9% of the disease producing bacteria are killed. In addition to killing the bacteria and infection, the laser also stimulates stem cells in the tissues to form new connective tissues, collagen and bone. Your body can then heal and rebuild these lost tissues.
At the end of treatment, a second laser is used to seal the tissues against the tooth root. This protects the pocket from germs and plaque getting back into the area while it is healing.
Ozone Cleaning and Disinfecting– Ozone is one of the most powerful natural oxidizing agents. It kills bacteria, disinfects, stops bleeding and stimulates wound healing. Used in a gas or liquid form, it has been shown to reduce bone loss and infection in 80% of periodontal disease areas, often significantly.
In nature, ozone (O3) occurs from atmospheric oxygen (O2). It develops as a result of ultraviolet light (sun) or electric spark discharge (thunderstorm, lightning) from air oxygen. In medicine, a special device generates a mini thunderstorm in a glass tube, and ozone occurs at the end of the tube. Being a gas, ozone is able to infiltrate the tissues, the smallest fissures, wounds, and gum pockets painlessly and without side effects.
Gum Irrigation– Once the pockets around the teeth are clean, they can be treated with liquid medications to help the tissues heal and regenerate. This procedure is called pocket irrigation and a variety of herbal and other health-stimulating irrigants can be used. I do not recommend using harsh antimicrobials such as Chlorhexidine, because of possible tissue damage.
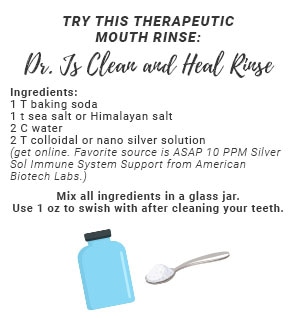
At Home Care after Periodontal Treatment
- Electric Toothbrush twice a day for two minutes
- Water Pik once a day for 2 minutes
- Use Herbal Mouthrinse for one minute (Tooth and Gum Tonic is recommended)
- Tongue Scraper every morning and night
Related: [How to Use A Tongue Scraper, And Why You Should Make It A Habit]
Nutrition and Supplementation for Gum Disease Treatment
Vitamins and minerals, particularly the fat-soluble vitamins A, D3, E, K2, are essential to gum and bone health. When a diet is devoid of minerals and high in sugar and processed foods, it causes the body chemistry to be out of balance.

The best way to get all of your vitamins and minerals is by eating lots of fresh fruit and veggies.
In particular, the imbalance of calcium and phosphorus leads to excess calcium in the blood and too little calcium available for the body to use.
In this situation, the body has to borrow calcium from somewhere to correct the imbalance. If there is not enough calcium for the essential organs to function, they will borrow it from the bone around the teeth.
This action sets up a weakened oral system that will quickly become infected. Although we see that infection and may conclude that gum disease is always an infection caused by bacteria, poor nutrition set the stage for that infection to occur.
[Related: Get Healthier Teeth And Gums With These 7 Foods For Oral Health]
Dietary Minerals Are Key
What can you do to prevent this mineral imbalance? Two things are key. You must either EAT or SUPPLEMENT minerals every day, and you must make sure your digestive system is ABSORBING those minerals.
Some signs that you aren’t getting enough minerals are sensitive teeth, achy joints and graying hair. If you are deficient, you will need to take a Fulvic and Humic Acid supplement like GreenSmoothieGirl’s Ultimate Minerals, and may need to work on your digestive system.
I've seen this delicate balance tip so many times in practice. A patient will have a perfect exam one visit, and six months later, will have gum disease. When we start to ask what's happened in their life in the last six months, we always hear about dietary changes, stress, perhaps illness, and always something that taxed their immune system.
Bone And Gum Tissue Can Heal
The good news is, I’ve also seen this in reverse. After addressing the causes of the disease, I’ve seen bone regrow and gum tissue heal. The body is a masterpiece and has the ability to heal if we provide the tools and materials it needs.
Supplement Recommendations:
- Vit D3/K2
- Omega 3 Fatty Acids
- Cell Salts - Calc Fluor, Calc Phos, Silicea
- Dr. Christopher's Complete Tissue and Bone
- Fulvic and Humic Minerals
- Zinc
Read next: What Causes Dry Mouth? Know the Symptoms and the Solutions

Sources
- Maxfield L, Crane JS. Vitamin C Deficiency (Scurvy) [Updated 2018 Aug 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 January. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493187
- American Academy of Periodontology. CDC: Half of American Adults Have Periodontal Disease. 2012. https://www.perio.org/consumer/cdc-study.htm
- Shangase SL, Mohangi GU, Hassam-Essa S, Wood NH (2013) The Association Between Periodontitis and Systemic Health: An Overview. SADJ 68: 8, 10-12.
- Gum Disease. National Institute of Dental and Craniofacial Research. 2017. https://www.nidcr.nih.gov/sites/default/files/2017-09/periodontal-disease_0.pdf
- Ahn J, Segers S, Hayes R (2012) Periodontal disease, Porphyromonas gingivalis serum antibody levels and orodigestive cancer mortality. Carcinogenesis 33: 1055-1058.
- Michaud DS (2013) Role of bacterial infections in pancreatic cancer. Carcinogenesis 34: 2193-2197.
- Whitmore SE, Lamont RJ (2014) Oral bacteria and cancer. PLoS Pathog 10: e1003933.
- Yao CS, Waterfield JD, Shen Y, Haapasalo M, Macentee MI (2013). In vitro antibacterial effect of carbamide peroxide on oral biofilm. J Oral Microbiol 5.
- Al-Katma MK, Bissada NF, Bourdeaux JM, Sue J, Askari AD (2007) Control of periodontal infection reduces the severity of active rheumatoid arthritis. J Clin Rheumatol 13:134-137.
- Nasr SH, Radhakrishnan J, D'Agati VD (2013) Bacterial infection-related glomerulonephritis in adults. Kidney Int 83:792-803.
- Chukkapalli S, Rivera-Kweh MF, Velsko IM, Chen H, Zheng D, Bhattacharyya I, et al. (2015) Chronic oral infection with major periodontal bacteria Tannerella forsythia modulates systemic atherosclerosis risk factors and inflammatory markers. Pathogens and Disease. 73.
- Louhelainen AM, Aho J, Tuomisto S, Aittoniemi J, Vuento R, et al. (2014) Oral bacterial DNA findings in pericardial findings. J Oral Microbiol 6: 25835.
- Wahid A, Chaudry S, Ehsan A, Butt S, Ali Khan A (2013) Bidirectional Relationship between Chronic Kidney Disease and Periodontal Disease. Pak J Med Sci 29: 211-215.
- Noble JM, Scarmeas N, Papapano PN (2013). Poor oral health as a chronic, potentially modifiable dementia risk factor: review of the literature. Curr Neurol Neurosci Rep 13: 384.
- Dzingute A, Pileicikiene G, Baltrusaityte A, Skirbutis G. Evaluation of the relationship between the occlusion parameters and symptoms of the temporomandibular joint disorder. Acta Med Litu. 2017;24(3);167-175.
- Oral Health Foundation. Jaw Problems and Headaches. Accessed November 17, 2018. https://www.dentalhealth.org/jaw-problems-and-headaches
Disclaimer: This article may contain affiliate links, which allow you to support our mission without costing you extra.
Posted in: Dental Health, Holistic Care