Periodontitis vs Gingivitis: Know the Differences & Warning Signs

Your gums are one of the most critical elements in a healthy mouth. They’re the oral equivalent of the foundation of your house: as long as the foundation is solid, the house is sound – but as soon as the foundation begins to shift or crack, the whole house could tumble down. Similarly, as soon as your gums start to deteriorate, you’re at risk for serious infection, bone loss, losing your teeth, and even disease.
In this article:
- How Gum Disease Begins
- Periodontitis vs. Gingivitis: What's the Difference?
- Periodontitis Treatment
- Preventing Gum Disease
How Gum Disease Begins

Plaque is bad for your gums and can lead to both gingivitis and periodontitis.
Gum disease develops the same way foundational issues usually do: with small changes that get increasingly worse until they cause serious issues.
It all begins with bacteria. Your mouth is actually filled with hundreds of types of bacteria¹, but only some of those are the dangerous types that lead to oral health issues.
When the bad type of bacteria swirls around in your mouth and lands on your teeth, it can stick and start to band together to form dental plaque. If that plaque isn't cleaned off within a few days, it calcifies and becomes tartar. This is a great place for more bacteria to congregate. Those bacteria eat the sugar and other foods you eat, and create acid that lands on the teeth and gums. The acids draw minerals out of the teeth and inflame the gums.
Bad for your teeth, obviously, but especially bad for your gums; plaque can lead to gingivitis and periodontitis.
Periodontitis vs Gingivitis: What’s the Difference?
You’ve probably heard several terms related to gum disease and may wonder about the difference between gingivitis and periodontitis. In these early stages when plaque build-up starts to harden, forming what’s known as tartar², your gums can become irritated and inflamed. That’s what’s known as “gingivitis.”
Symptoms of gingivitis³ include bad breath, along with effects on the gums like:
- tenderness
- a puffy or swollen appearance
- a dark red color
- bleeding gums
- actual pulling away from the teeth
At this point, symptoms aren’t too severe, and your teeth are still firmly anchored by bones, tissues, and ligaments in your jaw. Your house is still stable on the foundation, but there are warning signs of danger ahead.
Gingivitis can be treated by removing the accumulated plaque that has hardened into tartar with a professional cleaning4, regular brushing and flossing, and a healthy diet. If gingivitis is properly treated, it will not necessarily progress into the more serious gum disease known as periodontitis.
While the difference between gingivitis and periodontitis might start out as minimal, it’s an important distinction as it becomes more severe.
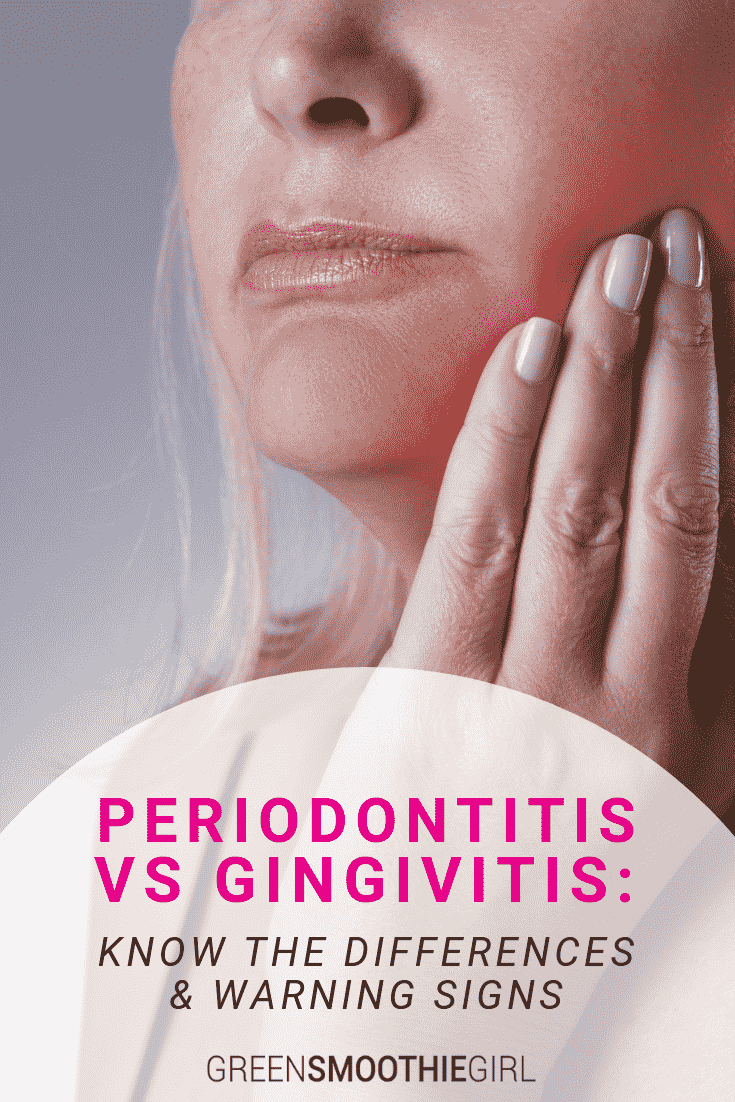
Periodontitis is a more advanced form of gum disease than gingivitis. Periodontitis officially begins when your gums get so inflamed by plaque and tartar accumulation that they start to pull away from your teeth¹. The bone holding your teeth is damaged, leading to bone loss. As your gums pull away and bone is lost, infected pockets start to form, like cracks forming in your foundation.
Periodontitis includes the same symptoms as gingivitis, but in its more advanced state, symptoms also include5:
- teeth that appear to be “longer” because gums have receded
- spaces that develop in between teeth
- pus or infected tissue near the teeth and gums
- loose teeth
- pain during chewing
- changes in your “bite” or tooth alignment
At this point, periodontitis can become a vicious cycle. As your body tries to fight the infection by moving away from the tartar, the pocket deepens and the tartar moves farther beneath the gum line, creating an even deeper infection that your body in turn tries to fight.
If this process continues untreated, the bones and tissues that hold your teeth will deteriorate and your gums will continue to worsen until your teeth become loose and then eventually fall out. Your house will crumble.
Even those who follow healthy oral hygiene routines and visit the dentist regularly can develop gingivitis that progresses into periodontitis. Other factors that play a role in the development of serious gum disease include:
- smoking and tobacco use5
- poor nutrition
- digestive problems that lead to malabsorption of nutrients
- family history
- pregnancy and increases in hormones
- diabetes and other chronic diseases
Because the bacteria predominant in periodontitis is also linked to heart disease and other conditions, periodontitis also raises risk6 for associated diabetes, arthritis, metabolic syndrome, high blood pressure, and some neurological diseases and cancers. With heart disease alone, periodontitis increases the risk 75%, and stroke by nearly the same.
Periodontitis Treatment

Dentists often start treating periodontitis with a deep cleaning.
Another difference between gingivitis and periodontitis is evident by the different ways in which they’re treated. Dentists often start treating periodontitis with a deep cleaning. During this process, they’ll use “scaling” to scrape the tartar off your teeth and “root planing” to buff out rough areas on your teeth where bacteria stick more easily. Medication – like a rinse, gel, or antibiotic – may also be prescribed. If none of these options effectively manages the advanced gum disease, surgery may be required.
If you do need periodontal surgery, there are some options that have shown to be effective at treating advanced gum disease. Your periodontist will help you choose which option has the most promising results for your specific situation and symptoms.
- During flap surgery, your periodontist will pull back your gums to scrape away tartar that’s accumulated in deep pockets. Your gums are then stitched back around your teeth and will heal to fit more tightly, helping to prevent tartar from getting beneath the gum line.
- If your gum disease has progressed to bone loss, a bone and tissue graft can help rejuvenate the bones and tissues that hold your teeth in place. Natural or man-made bone is placed in the area to encourage bone growth, and using guided tissue regeneration, a small piece of material placed in the area prevents the overgrowth of tissue, allowing space for new bone to form.
- New laser therapies are emerging that are the equivalent of flap surgery, but without pulling the gums back or requiring stitches. Check with your holistic dentist or periodontist if this treatment is available.
In some cases, neither flap surgery, laser therapy, nor bone and tissue grafts will be effective at treating advanced periodontitis. Your teeth may need to be extracted or may fall out on their own, leaving you with missing teeth or the need for costly implants or dentures.
Preventing Gum Disease
The difference between gingivitis and periodontitis can mean the difference between stopping gum disease before it becomes a serious issue and losing your teeth or developing disease. By managing your diet and the types of sugar you eat, brushing and flossing regularly, and scheduling regular dental cleanings to remove tartar, you can help to stop gingivitis from becoming periodontitis – and the more serious consequences that come with it.
Read next: Can Soda Dissolve Teeth? The Worst Drinks for Dental Health

Disclosure: This post may contain affiliate links that help support the GSG mission without costing you extra. I recommend only companies and products that I use myself.
SOURCES
- Loesche WJ. Microbiology of Dental Decay and Periodontal Disease. In: Baron S, editor. Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. Chapter 99. Available from: https://www.ncbi.nlm.nih.gov/books/NBK8259/
- WebMD, “What is Tartar: 6 Tips to Control Tartar” Retrieved from: https://www.webmd.com/oral-health/guide/tartar-dental-calculus-overview#1
- Mayo Clinic, “Gingivitis” Retrieved from: https://www.mayoclinic.org/diseases-conditions/gingivitis/symptoms-causes/syc-20354453
- National Institute of Dental and Cranialfacial Research, “Periodontal (Gum) Disease: Causes, Symptoms, and Treatments” Retrieved from: https://www.nidcr.nih.gov/OralHealth/Topics/GumDiseases/PeriodontalGumDisease.htm
- Mayo Clinic, “Periodontitis” Retrieved from: https://www.mayoclinic.org/diseases-conditions/periodontitis/symptoms-causes/syc-20354473
- Pallasch, Thomas J. DDS, MS, and Wahl Michael J., DDS, “Focal Infection Theory: Appraisal and Reappraisal” Journal of California Dental Association March 2000. 28 (3): 195
Posted in: Dental Health, Health Concerns












No comments found, but you can be our first!